Polyvagal Theory and Chronic Pain and Symptoms
By Tanner Murtagh, MSW, RSW
At our clinic, we utilize Polyvagal Theory to support clients in reducing their chronic pain or symptoms. In this post we’ll explore Polyvagal Theory, providing education on the nervous system, and how this relates to your neuroplastic pain and symptoms.
Our human bodies contain a built-in hierarchy of responses, meaning we shift between three systems depending on safety or danger. Our nervous system detects and interprets signals of either safety or danger and guides what system we shift into1.
The Parasympathetic Branch
Your parasympathetic branch consists of your vagus nerve, the 10th cranial nerve and the longest of the cranial nerves1, 2.
The vagus nerve facilitates bidirectional communication between the body and brain:
- 80% of safety or danger signals are sensory, meaning they come from the body and go to the brain.
- Only 20% of safety or danger signals are motor, meaning the messages come directly from the brain1, 2.
This is why safety starts in the body! While thinking and beliefs are important, we are greatly influenced by our nervous system state. To fully heal trauma, mental health problems, and chronic pain/symptoms, we need to regulate the nervous system. At our clinic we focus our treatment on this.
The vagus nerve travels from the brainstem at the base of the skull in 2 directions1, 2:
- Downward through the lungs, heart, diaphragm, and stomach.
- Upward to connect with nerves in the neck, throat, eyes, and ears.
The vagus nerve is split into two parts: the ventral vagal system and the dorsal vagal system.
The Dorsal Vagal System
Evolutionarily, this system is 500 million years old! The dorsal vagal system is unmyelinated, comes down the back of the body, and is located below the diaphragm1, 2.
The dorsal vagal system responds to signals of extreme danger, causing us to freeze, disconnect, dissociate, feel numb or depressed, and protect ourselves by going into a state of shutdown and collapse1, 2.
The Ventral Vagal System
Evolutionarily, this system is 200 million years old! The ventral vagal system is myelinated, comes down the front of the body, and is located above the diaphragm1, 2.
The ventral vagal system responds to signals of safety, allowing us to feel socially connected, engaged, and safe. Part of the ventral vagal system is the social engagement system which controls facial expression, social gaze, middle ear muscles, ingestion, vocalizing, swallowing, breathing, orienting, and social gesturing1, 2.
The Sympathetic Branch
Evolutionarily, the sympathetic system is 400 million years old! It is found in the midsection of the spinal cord1, 2.
The sympathetic system mobilizes us for action, responding to signals of danger by triggering our fight or flight response. But, it’s more than just fight or flight! It provides energy to live – excitement, play or passion1, 2.
Shifting Within the Autonomic Nervous System
The autonomic nervous system shifts between ventral vagal, sympathetic, and dorsal vagal based on neuroception1, 2.
- Signals of safety → ventral vagal activation (connected, safe, social, calm) 1, 2
- Signals of danger → sympathetic system activation (mobilize to fight or flee) 1, 2
- Often, taking action helps us restore safety and shift back to the ventral vagal system
- High, inescapable, and persistent danger → dorsal vagal activation (freeze, shut down, and collapse to survive) 1, 2
- This may also be a helpful survival option!
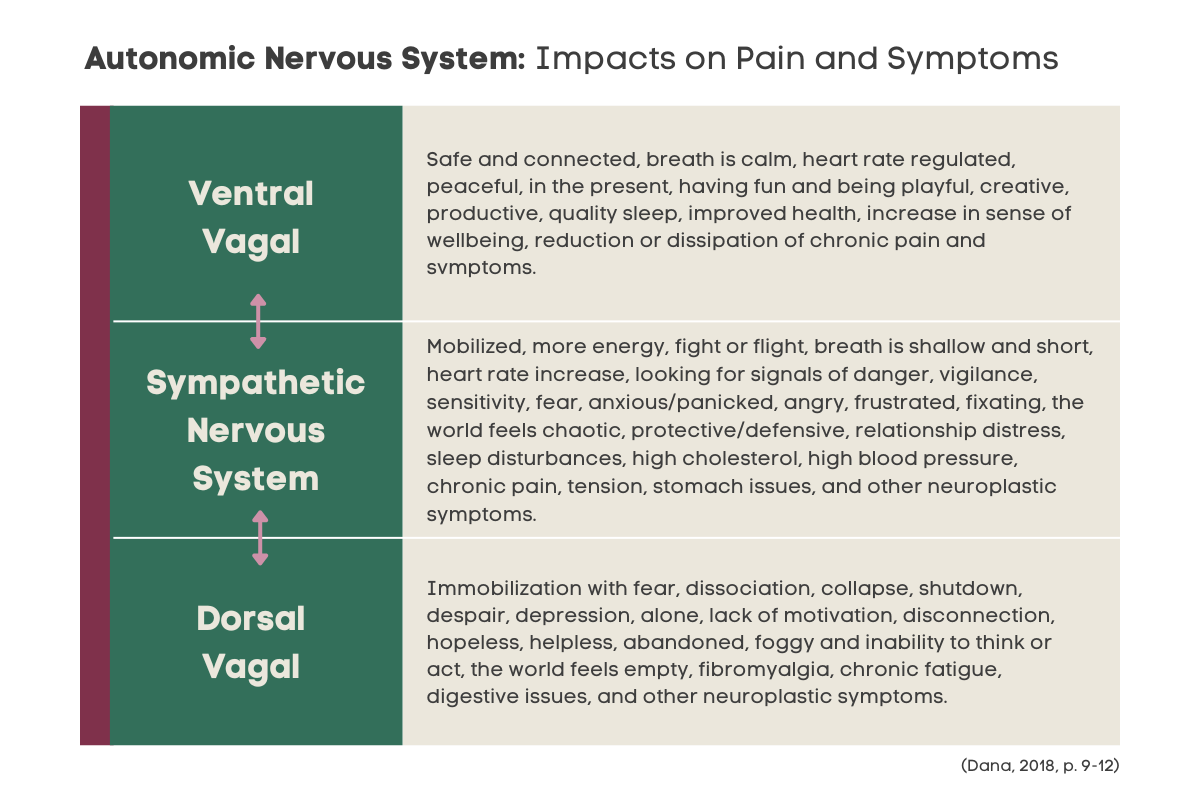
This chart shows how we typically experience the three different systems and how they can impact pain and symptoms:
An important note: Briefly shifting into the sympathetic or dorsal vagal systems is healthy as long as we’re able to shift back to safety with ease. It’s when we’re dysregulated for prolonged periods of time that our nervous system becomes sensitized, triggering and perpetuating chronic pain and symptoms 1, 2.
A key focus for our therapists when collaborating with clients is to assist their nervous system in accurately recognizing signals of safety and danger, both internally and externally. This allows the nervous system the ability to shift more easily to a ventral vagal state after they experience stressors. We support clients in learning how to connect with their body and understand what state they are in. This is a vital step in having a client’s chronic pain and symptoms reduced.
To begin your healing, book a free 20-minute consultation with one of our therapists:
Dana, D. (2018). The polyvagal theory in therapy: Engaging the rhythm of regulation. W W Norton & Co.
Porges, S. W. (2019) Clinical Applications of the Polyvagal Theory.
Dana, D. (2019). 2-Day Workshop: Polyvagal Theory Informed Trauma Assessment and Interventions